|
At times we all find ourselves struggling with extremes within our lives: going from unrestricted eating to strict diets; drinking alcohol to excess then stopping drinking for a period of time; exercising then not exercising; working non-stop then losing motivation. Extremes are part of being human and are a normal part of life. Extremes become problematic is when you they start to become harmful to yourself or those around you. In DBT we think about how we can 'walk the middle path,' holding the wisdom at one end of the extreme whilst also acknowledging the truth in the other end.
In DBT, we acknowledge that two things that might seem like opposites can both be true. For example, on a day with a clear blue sky, the sea is blue; and the sea is also colourless. Both aspects of this are true and it may seem possible to acknowledge the truth in both. Yet for things that directly affect us, it can be harder to hold onto both ends of the spectrum. A thought such as "I hate my job" can throw us into despair and strong emotion states rather than exploring whether there is any truth left at the end of loving your job. Putting this into action in our lives is one of the central aspects of DBT. Simple ways to manage extremes in thinking by being more dialectical includes:
There are many other ways to use dialectics to manage extremes. If you'd like to explore how DBT can help you then please contact our service.
0 Comments
Mindfulness is one of the core modules in the skills component of Dialectical Behaviour Therapy (DBT) and forms the basis of various other cognitive behavioural approaches (e.g. mindfulness based cognitive therapy, Acceptance and Commitment therapy). Mindfulness is derived from Eastern, Buddhist traditions but is utilised in psychotherapy as a way of paying attention, on purpose to the present moment in a non-judgemental manner (definition adapted from Jon Kabat-Zinn). So what does this really mean? For me, mindfulness is about knowing my mind; it’s about being familiar with where my mind wanders to when I’m worried, frightened, sad or even happy. Practising mindfulness has enabled me to be kinder towards myself as I recognise the habitual patterns of my mind rather than taking my thoughts seriously, as if they are reflections of reality. Sometimes I am even able to greet my thoughts as though they are old acquaintances, with ideas I don’t necessarily agree with, but recognising the familiar patterns of their utterances with a degree of fondness.
I practise mindfulness both for my own personal benefit and in order to be an authentic DBT therapist (indeed, I try to practise all the skills). It takes effort and practice and sometimes the abstract nature of a practice (e.g. focusing on an object in a moment) can seem somewhat removed from the essence of what it is I am hoping to cultivate in my clients. I am aware of the criticisms of mindfulness from purists and those that follow the traditional components of the practices but I believe mindfulness, even in its sanitised, adapted format, has much to offer. Slowing down, focusing, noticing and for once, not striving, is alien in our culture. Learning to just “be” rather than always “doing” is a lesson in itself. Alongside the benefits for the general population, the people who access therapy with our service struggle with intense emotions, distress and pain that is hard for most people to imagine. The notion of mindfulness is thorny and difficult. We ask people to accept and be at one with their pain, to let go of expectations that pain will go away and instead just notice it. This is the polar opposite of what most people (in our service or not) do when they experience intense emotions; most people run away from pain, doing anything they can to quieten it. Mindfulness invites people to take a different relationship with the difficult experiences they face. Instead of judging emotions, wanting them to go away or trying to avoid them, mindfulness asks individuals to just notice the emotion or the breath. This simple idea is not one easily accepted by the thinking mind but one that, with practice, can be hugely beneficial. In allowing yourself to be present and notice what it is you are experiencing without the thinking mind chattering away and directing your action, you have more of a choice about how you are going to respond. Indeed, the emotions may be different to the picture painted by the thinking mind and you might find that allowing emotions simply to be changes them. Utilising this skill when it’s most needed though requires practice and practice can be hard. Finding practical strategies to remind yourself as well as committing to giving mindfulness a go can be helpful ways of starting to integrate it into your life. If you’re interested in learning more about mindfulness, there are many resources on the internet and guided meditations on youtube. Mindfulness as part of DBT has specific components which we will blog about too. If you are interested in accessing DBT or a DBT-informed approach, please contact us ([email protected]). At the peak of emotional intensity, you can be blinded by your distress and unable to think through logical options. This often leads people to act in impulsive and harmful ways to reduce the distress in the moment (e.g. self-harming) but creates a vicious cycle in which self-harm becomes the only option to reduce distress. DBT helps teach different skills to understand, manage and tolerate emotions. One such skill is the TIP skill. This skill is one to be used when you are in the eye of the emotional storm and when others skills simply would not work. There is a great deal of evidence and science behind each skill, some of which I will explore in this blog.
Before I explain the TIP skills, it is important to explain why the skills work. The TIP skills work on the parasympathetic nervous system. Put simply, the nervous system is made up of two systems which work in opposite directions from one another. The sympathetic nervous system is activating; it triggers the fight or flight response which sets off a whole host of physical, emotional and cognitive processes. The parasympathetic nervous system does the opposite: it slows you down and increases thoughtful, considered and emotionally attuned responses. The TIP skills act on the parasympathetic nervous system to help alleviate the intensity of the emotions and distress. What is important to remember here is that impacting on our physiology can have a huge impact on our emotions and thoughts. An interesting example of this is described by Amy Cuddy in her TED talk about how we hold our body changes our emotional, cognitive and even biochemical state (https://www.ted.com/talks/amy_cuddy_your_body_language_shapes_who_you_are another important thing she talks about here is faking it to make it, something we will try to explore in future blogs). The T stands for Temperature and involves tipping your face into cold water or putting a cold flannels onto your face whilst briefly holding your breath. This induces something called the dive reflex which is a naturally occurring process of slowing the heart rate when immersed in cold water without oxygen. Linehan (2015) suggests that this skill is helpful in states of high emotional arousal as well as times when you cannot sleep due to ruminative thoughts or during dissociative episodes. Linehan (2015) warns that this skill should not be used if you have a heart condition and that the effects are short lived therefore it is important to follow up immediately with an activity that continues to reduce arousal, is distracting or problem solving. Intense exercise is the next skill. This means doing any intense aerobic exercise for 20 minutes; running, cycling, dancing, jumping, anything that gets your heart rate up! This can lead to a decrease in negative mood and ruminative thoughts. Linehan (2015) asserts that emotions activate the body and call for action. This often leads to destructive behaviour in people with a personality disorder however; intensive exercise re-regulates the body leading to reduced emotional arousal. This skill can be used when you are agitated or angry to help bring the emotion down so that you can engage in wise mind activities. The P stands for paced breathing (Linehan, 2015). This means slowing your breathing rate to 5-6 breaths per minute. Linehan (2015) refers again to the sympathetic (activating) and parasympathetic (slowing) system to explain why this works. She explains that the sympathetic system becomes active when we breathe in and the parasympathetic system activates when we breathe out (Linehan, 2015). Thus, it is important to breathe out for longer than we breathe in (e.g. breathe in for 4 counts and out for 6 counts). The final P (not included in the acronym) is for paired muscle relaxation. For the reasons described above, this involves pairing relaxing the muscles as you breathe out. There are numerous resources online to illustrate how to do this e.g. progressive muscle relaxation. However, it is important to note that the use of the breath can augment the calming effects of this exercise. Linehan (2015) argues that together, these skills are just as effective at reducing the intensity of emotions as destructive behaviours such as self-harm. As part of our DBT service, we work to develop these skills with the individuals we work with. Changing habitual patterns such as self-harm is very challenging, particularly when alternatives don’t seem as effective or helpful in reducing the overwhelming intensity of emotions in the moment. Practicing these skills, even when not in the eye of the emotional storm is very important to ensure the skills are readily available when most needed. If you are interested in accessing DBT treatment, please contact us ([email protected]) to explore options with our service. References LInehan, M.M. (2015). DBT skills training manual. Guilford Press.  We are seeing more and more self-harming amongst young people, possibly in response to increased cyberbullying, through increased exposure to information, images and possibilities available through social media and the world wide web. A friend spoke to me as a parent of a teenage girl. She became aware of her daughter cutting her legs only when she placed her hand on her leg whilst driving and her daughter winced. My friend described feeling out of her depth, very distressed herself with very little idea of how to approach the issue. She remembered being terrified of making things worse. This blog identifies some skills from Dialectical Behaviour Therapy (DBT) Skills Training for use to assist parents and young people who may find themselves facing similar challenges. When a person hurts themselves it can be understood as a way of dealing with very difficult feelings, painful memories or overwhelming situations and experiences. It can be something young people turn to when they feel they have no other option. Responses given by young people about why they self-harm are likely to be all different, individualised and person specific but can include:-
Difficulties regulating or managing emotions in young people can sometimes be in response to their experience of invalidation. Busy, committed lifestyles can sometimes lead to young people’s communications of emotion going unnoticed, or their attempts to communicate triggers an extreme response from care givers. Because the message a young person is trying to communicate is important, things can quickly escalate. VALIDATION
INVALIDATION
 What to do then ? When parents are facing crisis situations, where a child is engaging in dangerous potentially life threatening acts, e. g cutting themselves or taking overdoses, it is difficult to know what to do. Efforts to try to help, are understandably motivated by anxiety or fear and an overwhelming desire to keep their loved one safe. The emotional temperature of the family unit often rises and it isn’t always possible to make measured reasoned responses. Useful things to bear in mind if the situation allows for it:
DBT seeks to find the middle ground between acceptance and change. In crisis situations it’s difficult to remember the acceptance part because the motivation to make things better, and halt the self-harm is strong. In this situation the ability and willingness to accept in the moment is the vehicle of change in the longer term. DBT Acceptance skills are Mindfulness , Distress Tolerance. DBT Change Skills are Emotional Regulation, Interpersonal Effectiveness. Initially it could be useful to use some Mindfulness skills with your child: Observe-Just Notice Notice body sensations, pay attention, practice wordless watching. Describe-Put words on the experience. When a feeling or thought arises, describe it in your mind. Label what you observe. Unglue your interpretations and opinions from the facts. Describe the facts. Who, what , where, when. Interpersonal Effectiveness Skills Where there is a need to improve communication, open or maintain a dialogue. Here the skill of validation could be applied. VALIDATION Validation means finding the truth in another person’s perspective or situation and verifying the facts of a situation. Acknowledge that a person’s emotions, thoughts and behaviours have causes and are therefore understandable. This does not necessarily mean agreeing with the other person but means accepting and validating the emotions in the moment as they are. It is important to validate (rather than deny) a person’s feelings as being true, accurate and always acceptable (even if sometimes their expression and management of emotions may be hard to understand) Why Validate?
- The facts of a situation. - A persons experiences, feelings/emotions ,beliefs ,opinions ,or thoughts about something. - Suffering and difficulties. Remember Validation is not necessarily agreeing. Validation doesn’t mean you like it. Only validate the valid! If you would like help and support either with self-harm or someone close to you who is engaging in such behaviour, please contact us or check out our consultation package for further individualised bespoke support and advice. References DBT Skills Training Handouts and Worksheets –Marsha M Linehan second edition 2015 Guilford Press. Cognitive Behavioural Treatment of Borderline Personality Disorder-Marsha M Linehan 1993 Guilford Press. Mind Understanding Self Harm Publication/pdf Keeping Children ,Young People and Families safe booklet-Safety Net 2013 AuthorAnne Francis is a Dialectical Behaviour Therapist and Mental Health Nurse. She has expertise in, and extensive experience of, working with adults and young people who self harm and is part of the Brighter Horizons Brighton DBT team. Why taking a bath doesn't help: Developing strategies to manage emotions when they become intense2/27/2017 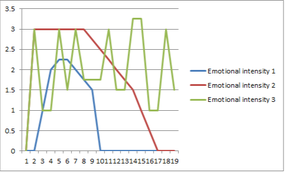 Skills to manage emotional intensity often need to be adapted according to the type of emotion experienced and the intensity. Once triggered, emotions often quickly rise and then fall naturally back to baseline (blue line). For someone with mental health problems such as borderline personality disorder, the intensity of the emotion is often higher, longer lasting and the return to baseline is much slower (red line). Sometimes people with mental health problems will use harmful means to quickly bring the intensity of their emotions down but overall these strategies leave them more vulnerable to further emotional intensity episodes and more reliant on harmful means to regulate their emotions (green line). Often people we work with say they're told to "have a bath" to manage the intensity of their feelings. This can be the worst thing to be told; most people (mental health problems or not) are unlikely to be able to relax in the bath at the peak of their stress. However, for some people a bath can be a useful soothing activity once the emotion starts to come down. So it's about choosing an action appropriate to the intensity of the emotion. At the peak of distress, often it is most important to think of ways of reducing your physiological (body) arousal. This could be by using methods to regulate your breathing (taking deep breaths and focusing only on your breathing in the moment), slowing your movements in a deliberate manner, talking yourself through what you are doing physically in the moment or doing the opposite of your urges. If you've learned to cope with emotions by harming yourself in some way then trying something different can feel difficult and not as immediately calming in the short term as your previous strategy. Sometimes people describe needing an intense outlet for their feelings. Snapping an elastic band on your wrist, plunging your face briefly into ice cold water or using a marker pen to make lines on your arm are all strategies to try. In the medium/long term, acting in accordance with the person you want to be will outweigh the seemingly immediate but short term effects of harmful behaviour. It is also important to practice these skills on a regular basis and think about what strategies might work at the different levels of your own emotional peaks. Writing ideas down can help as when the wave of emotional intensity hits it can be hard to make decisions about what to do or try. If you have ideas or things that you've tried, please do comment on this blog to share with others. The ability to soothe intense emotions is an important skill but one that people often experience a great deal of difficulty with. Our mind throws lots of reasons why we shouldn't prioritise activities that soothe our senses. Paul Gilbert (The Compassionate Mind, 2009) argues that effectively managing emotions requires the development and balance of 3 basic emotion systems:
However, an inability to soothe ourselves can lead to emotional intensity that feels out of control, on going mental health problems (depression, anxiety) and feelings of stress. It is vital that we attend to our 3 basic emotion regulation systems in order to keep our emotions balanced. You can learn to self soothe and below are a number of strategies of things to try. The first step in self-soothing is mindfulness (we will blog about this in a separate post). In brief, mindfulness is the skill of noticing and being present in the moment without judgement. It can help to notice the obstacles our brain throws at us when we attempt to self-soothe. Notice these without judgement, our brains have well trodden neural pathways so these negative evaluations and criticisms will inevitably show up, but try to just notice them and let them pass, like a cloud in the sky. The best way to learn to self soothe is to think about the 5 senses and how you can soothe each sense. Hearing: Soothing music or sounds (nature) Touch: Mindfully applying hand cream, taking a bath Vision: Dim lighting, candles, soothing colours Smell: Scented candles, clean clothes or bedsheets Taste: Sweet tastes (chocolate) Combining senses can help further develop your ability to self-soothe. It is important to practice this skill, even when you don't feel the need to be soothed. Self-soothe can be particularly beneficial either when you notice your emotional intensity/stress rising or when you are coming down from an episode of intensity or stress. Often at the peak of distress, self-soothe can be very difficult to achieve. We will write other blog posts on what to do when you are at the peak of emotional intensity focusing on strategies to reduce the levels of distress in helpful ways. Development of DBTLinehan and her research team initially applied standard Cognitive Behavioural Therapy techniques when working with their suicidal client group. However, during treatment they observed numerous problems with its use.
Three factors were particularly problematic and consistently influenced treatment outcomes:
Adding Validation and Dialectics to CBT. Acceptance-based interventions, frequently referred to as validation strategies, were added. Adding these communicated to the clients that they were both acceptable as they were and that their behaviours including those that were self-harming, made real sense in some way. The emphasis on acceptance did not exclude the emphasis on change. Clients must also change if they want to build a life worth living. Thus ,treatment focuses on both acceptance and change. Dialectical strategies gave the therapist a means to balance acceptance and change in each session .They also serve to prevent client and therapist from becoming stuck with thoughts, feelings and behaviours that can occur when emotions run high in the therapy setting with those with BPD diagnosis. Dialectical strategies and a dialectical world view, with its emphasis on holism and synthesis, enable the therapist to blend acceptance and change in a manner that results in movement, speed, and flow in individual sessions and across the entire treatment. Functions and Modes. Linehan (1993) hypothesizes that any comprehensive psychotherapy must meet five critical functions. The therapy must: a) enhance and maintain the client’s motivation to change; b) enhance the client’s capabilities; c) ensure that the client’s new capabilities are generalized to all relevant environments; d) enhance the therapist’s motivation to treat clients while also enhancing the therapist’s capabilities; and, e) structure the environment so that treatment can take place. Standard outpatient DBT meets these functions by offering Individual therapy sessions, skills training groups, skills coaching and a therapist consultation group. It is typically the individual therapist who maintains the client’s motivation for treatment, since the individual therapist is the most salient individual for the client. Skills are acquired, strengthened, and generalized through the combination of skills groups, phone coaching (clients are instructed to call therapists for coaching prior to engaging in self harm), in vivo coaching, and homework assignments. Therapists’ capabilities are enhanced and burnout prevented through weekly consultation team meetings. The consultation team helps the therapist stay balanced in his or her approach to the client, while supporting and cheerleading the therapist in applying effective interventions. Finally, the environment can be structured in a variety of ways, say by the client and therapist meeting with family members to ensure that the client is not being reinforced for maladaptive behaviours or punished for effective behaviours in the home. Stages and Targets. DBT also organizes treatment into stages and targets and, with very few exceptions, adheres strictly to the order in which problems are addressed. The organization of the treatment into stages and targets prevents DBT being a treatment that, week after week, addresses the crisis of the moment. Further, it has a logical progression that first addresses behaviours that could lead to the client’s death, then behaviours that could lead to premature termination of therapy, to behaviours that destroy the quality of life, to the need for alternative skills. In other words, the first goal is to insure the client stays alive, so that the second goal (staying in therapy), results in meeting the third goal (building a better quality of life), partly through the acquisition of new behaviours (skills). In short, we have just described the targets found in Stage I. In Stage II, DBT addresses the client’s inhibited emotional experiencing. It is thought that the client’s behaviour is now under control but the client is suffering “in silence”. The goal of Stage II is to help the client move from a state of quiet desperation to one of full emotional experiencing. This is the stage in which post-traumatic stress disorder (PTSD) would be treated. Stage III DBT focuses on problems in living, with the goal being that the client has a life of ordinary happiness and unhappiness. Linehan has posited a Stage IV specifically for those clients for whom a life of ordinary happiness and unhappiness fails to meet a further goal of spiritual fulfilment or a sense of connectedness of a greater whole. In this stage, the goal of treatment is for the client to move from a sense of incompleteness towards a life that involves an ongoing capacity for experiences of joy and freedom. Adapted from the behavioural tech website. |
Archives
October 2022
Categories |
DBT
Blog
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
 RSS Feed
RSS Feed
