Background information on DBT
Why is it called 'Dialectical' Behaviour Therapy?
A dialectic two apparently opposite positions. The aim of dialectical behaviour therapy is to help individuals find the middle ground between the opposing emotional, cognitive and behavioural experiences within their lives. When developing DBT, Marsha Linehan found that dialectical thinking formed a consistent pattern for people with Borderline Personality Disorder. She found that acknowledging these dialectics and helping clients to find the middle ground between the extremes was a helpful and effective way of working. The dialectic forming one of the central components of DBT is acceptance and change. Clients are accepted as they are and their behaviours, including self-harm, are accepted and understood as making absolute sense. On the other side of this, there is an emphasis on change and an understanding that clients must make real changes in order to build a life worth living.
What is different about DBT compared with other therapies?
DBT draws from standard Cognitive Behavioural Therapy approaches but differs in several important ways. The dialectical component outlined above is one way in which DBT differs from other therapies. In addition, DBT was developed with a knowledge that therapy must be focused on areas important to the client and draw on their motivation to change, enhance and build on the skills that a client comes into therapy with, help to generalise the skills developed within therapy across all context of a clients' life and ensure that the therapist and environment are supported in a way that facilitates successful treatment.
Why was DBT developed?
Linehan and her research team initially applied standard Cognitive Behavioural Therapy (CBT) techniques when working with their suicidal client group. During treatment they observed numerous problems with its use. Three factors were particularly troublesome and consistently influenced treatment outcomes:
What are the key components of DBT?
Standard outpatient DBT offers individual therapy sessions, skills training groups, skills coaching and a therapist consultation group. Excellent practice also involves those around the client to ensure they are supporting the client to utilise their skills in adaptive ways.
How is DBT arranged?
DBT also organises treatment into stages and targets which decide the order in which issues are addressed. The predetermined order of treatment priorities is particularly important given the difficulties experienced by clients with a Borderline Personality Disorder diagnosis. Thus, rather than focusing on the most recent crisis, the treatment programme ensures that the first priority is addressing life threatening behaviours. The next stage in the programme focuses on behaviours that could interfere with the therapeutic relationship and successful outcome of treatment. Behaviours that impact on a clients' quality of life are the next focused and finally, DBT focuses on building alternative skills. Together, these form the key components of stage 1 of the DBT treatment programme.
Traditionally, after stage 1 of the treatment programme, clients may feel the need to go onto further therapy to address residual symptoms such as those associated with specific trauma experiences. Many clients choose to only complete stage 1 of the therapy as this helps build meaningful and lasting change.
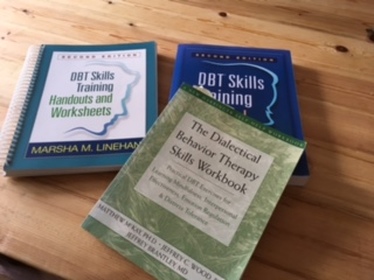
DBT Skills Training
Four DBT skills are taught primarily in the skills group sessions but may be revised or practiced in individual therapy sessions. The skills training includes:
A dialectic two apparently opposite positions. The aim of dialectical behaviour therapy is to help individuals find the middle ground between the opposing emotional, cognitive and behavioural experiences within their lives. When developing DBT, Marsha Linehan found that dialectical thinking formed a consistent pattern for people with Borderline Personality Disorder. She found that acknowledging these dialectics and helping clients to find the middle ground between the extremes was a helpful and effective way of working. The dialectic forming one of the central components of DBT is acceptance and change. Clients are accepted as they are and their behaviours, including self-harm, are accepted and understood as making absolute sense. On the other side of this, there is an emphasis on change and an understanding that clients must make real changes in order to build a life worth living.
What is different about DBT compared with other therapies?
DBT draws from standard Cognitive Behavioural Therapy approaches but differs in several important ways. The dialectical component outlined above is one way in which DBT differs from other therapies. In addition, DBT was developed with a knowledge that therapy must be focused on areas important to the client and draw on their motivation to change, enhance and build on the skills that a client comes into therapy with, help to generalise the skills developed within therapy across all context of a clients' life and ensure that the therapist and environment are supported in a way that facilitates successful treatment.
Why was DBT developed?
Linehan and her research team initially applied standard Cognitive Behavioural Therapy (CBT) techniques when working with their suicidal client group. During treatment they observed numerous problems with its use. Three factors were particularly troublesome and consistently influenced treatment outcomes:
- Clients receiving CBT found the continuous focus on change invalidating. Clients responded by withdrawing from treatment, by becoming angry, or by vacillating between the two. This resulted in a high drop out rate. This suggested that standard CBT was not an appropriate model for people diagnosed with BPD.
- Clients unintentionally positively reinforced their therapists for ineffective treatment while punishing their therapists for effective therapy.
- The volume and severity of problems presented by this particular client group made it impossible to use standard CBT which generally focuses on the problems experienced in the week between therapy sessions. Individual therapists did not have time to both address the problems presented by clients – suicide attempts, urges to self-harm, urges to quit treatment, noncompliance with homework assignments, untreated depression, anxiety disorders, etc, — and have session time devoted to helping the client learn and apply more adaptive skills.
What are the key components of DBT?
Standard outpatient DBT offers individual therapy sessions, skills training groups, skills coaching and a therapist consultation group. Excellent practice also involves those around the client to ensure they are supporting the client to utilise their skills in adaptive ways.
How is DBT arranged?
DBT also organises treatment into stages and targets which decide the order in which issues are addressed. The predetermined order of treatment priorities is particularly important given the difficulties experienced by clients with a Borderline Personality Disorder diagnosis. Thus, rather than focusing on the most recent crisis, the treatment programme ensures that the first priority is addressing life threatening behaviours. The next stage in the programme focuses on behaviours that could interfere with the therapeutic relationship and successful outcome of treatment. Behaviours that impact on a clients' quality of life are the next focused and finally, DBT focuses on building alternative skills. Together, these form the key components of stage 1 of the DBT treatment programme.
Traditionally, after stage 1 of the treatment programme, clients may feel the need to go onto further therapy to address residual symptoms such as those associated with specific trauma experiences. Many clients choose to only complete stage 1 of the therapy as this helps build meaningful and lasting change.
DBT Skills Training
Four DBT skills are taught primarily in the skills group sessions but may be revised or practiced in individual therapy sessions. The skills training includes:
In summary DBT is an effective, evidence-based treatment model which uses a range of Cognitive Behavioural strategies and mindfulness skills to enhance emotional and behavioural regulation, reduce self-harming and suicidal behaviours, and improves social functioning and quality of life.
|
Interpersonal effectiveness (7 sessions) teaches effective strategies for asking for what you need, saying no, and coping with interpersonal conflict. Because individuals with Borderline Personality Disorder and related difficulties often experience relationships that are chaotic, intense, and unstable, this module teaches skills for maintaining balanced interpersonal relationships.
|
